For some people suffering from illnesses such as schizophrenia and substance use disorder – previously referred to as “substance abuse” – making the right choices can be extremely difficult.
In fact, many mental illnesses feature problems with cognition (thinking and comprehension), including depression and bipolar disorder. Decision-making ability varies in healthy people, too, sometimes as a consequence of differences in genetics.
What’s happening in the brains of these people that puts them on unequal footing to the rest of us?
Even simple decisions are complex
It’s important to note in day-to-day situations, there’s often no distinctly “right” or “wrong” choice to be made. However, some choices do result in healthier or more productive outcomes for us and those around us.
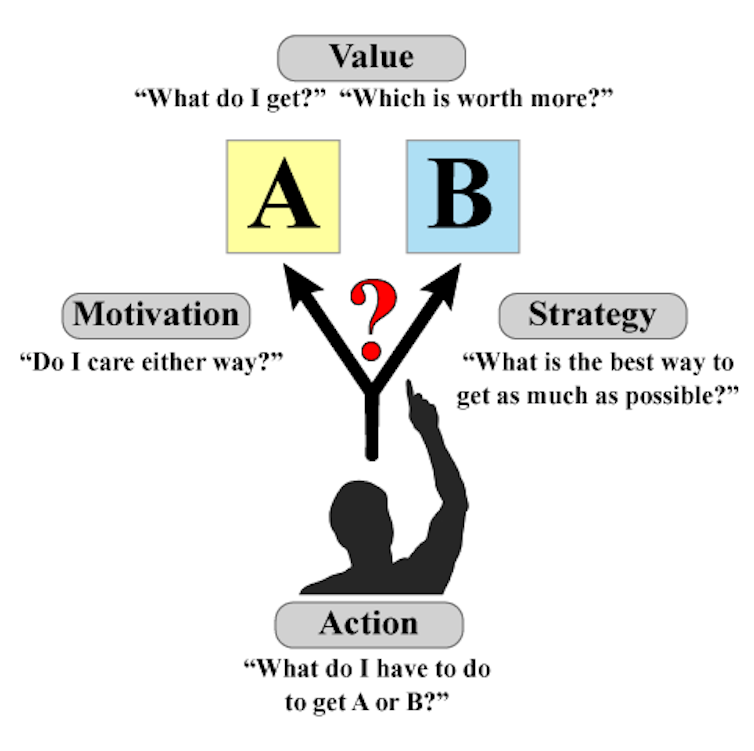
Our brains carry out a suite of complex processes when making decisions. And there are four important factors in each decision we make: value, motivation, action and strategy.
- Mapping health risks for people with mental disorders
- Researchers recognised for expanding knowledge of schizophrenia
- Research bears fruit for schizophrenia patients
When choosing between two options, say A and B, we first need to understand which choice will be more rewarding, or provide more value. Our personal motivation to attain this reward then acts to bias which option we choose, or whether we make a choice at all.
Understanding what action is required to obtain A, or B, is also important. Combining all this information, we try to understand which strategy will maximise our rewards. And this lets us improve our decision-making ability over time.
Connections interrupted by mental disorders
We refer to our personal history and past experiences to guide our future choices. But mental disorders often cause problems in the decision-making process.
Research shows people with schizophrenia can have trouble understanding the relationship between their actions and the outcomes. This means they might keep selecting A, even if they know it’s no longer as valuable as B.
They’re also more willing to adopt strategies based on less information, in other words “jump to conclusions”, about outcomes.
Substance use disorder, particularly with stimulants such as methamphetamine or cocaine, often leads to people getting stuck when certain outcomes change.
For example, if we reversed all the street lights so red meant “go” and green meant “stop” without telling anyone, most people would get an initial shock but would eventually alter their behaviour.
People with stimulant dependence, however, would take longer to learn to stop on the green light – even if they kept getting into car accidents. This is because excessive stimulant use impacts regions in the brain that are crucial to adapting to changing environments.
How the brain decodes each decision
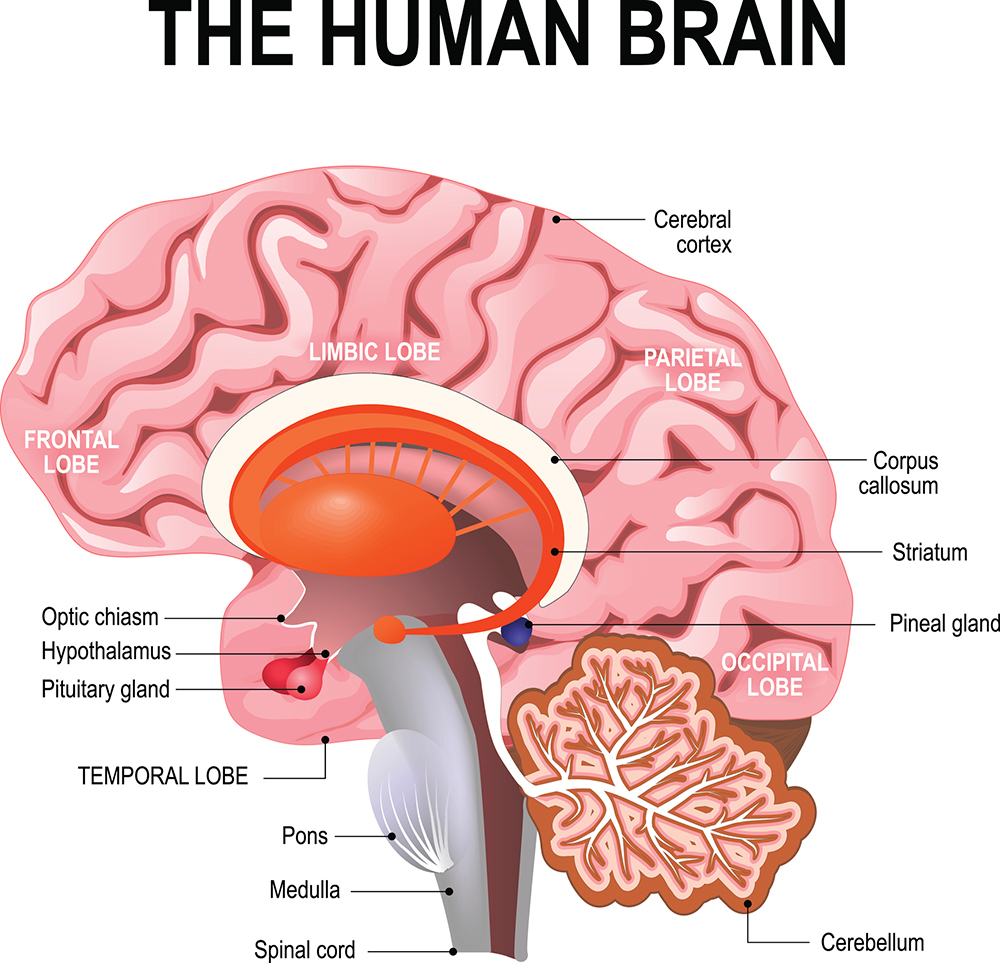
The human brain contains multiple circuits (like pathways) and chemical messengers called “neurotransmitters”. These are responsible for guiding the processes discussed above.
The decision-making circuits commonly associated with schizophrenia and substance use disorder include areas of the “cortex” – the outer part of our brain important for complex thought (especially the frontal lobe) – that “talk” to hub areas such as the “striatum”. The striatum lets us select and then initiate an action to achieve a specific goal.
Different cortical areas are used to compute different processes in the brain. The prefrontal cortex helps us understand when a strategy needed for success changes. So, if we replaced all the traffic lights with sirens, the prefrontal cortex would help us realise this and adjust.
When the anticipated outcome of a choice changes (such as if A was better, but then suddenly B became better), the orbitofrontal cortex helps us identify this. Similarly, the striatum is key for anticipating what an outcome will be and when we will get the reward.
Dopamine helps make choice a reality
Extensive research efforts have found the brains of people experiencing schizophrenia function differently in multiple areas. It’s believed this could contribute to decision-making problems.
For the psychotic symptoms observed in schizophrenia (such as hallucinations and delusions), alterations in the neurotransmitter dopamine are important. Dopamine is a chemical in the brain that’s key for anticipating rewards, making decisions and controlling the physical actions necessary to act on our choices.
In our research, we’ve argued increases in dopamine in the striatum may cause problems with how the brain integrates information from the cortex, resulting in decision-making difficulties. However, this may only be the case in some individuals.
Stimulants also cause excessive dopamine release. They can alter the balance between goal-directed behaviours, which are flexible and respond to environmental changes – and habits, which are automatic and hard to break.
Usually, when we learn something new our brain keeps adapting and incorporating new information. But this is slow and cognitively demanding. Substance dependence can accelerate a person’s progression to habitual behaviour, wherein a set strategy or response become ingrained.
This then makes it hard to stop seeking drugs, even if the individual no longer finds them enjoyable.
How to help people make better decisions
Unfortunately, problems with cognitive ability are hard to treat. There are no medications for schizophrenia or stimulant dependence shown to reliably improve cognition. This is a consequence of the human brain’s complexity.
That said, there are ways we can all improve our memory and decision-making, which may also help those with mental illnesses causing cognition problems.
For instance, cognitive remediation therapy is a behavioural approach that trains the brain to respond to certain situations better. For people with schizophrenia, it may improve visual memory and perhaps more complex decision-making.
Not being able to navigate decisions day-to-day is one of the most debilitating aspects of disorders that impact cognition. This leads to difficulties in maintaining work, keeping friends and leading a fulfilling life.
We need more research to understand how different brains make different decisions. Hopefully then we can improve the lives of those living with mental illness.
James Kesby, UQ Amplify Researcher, The University of Queensland and Shuichi Suetani, Psychiatrist, Queensland Brain Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.

