About
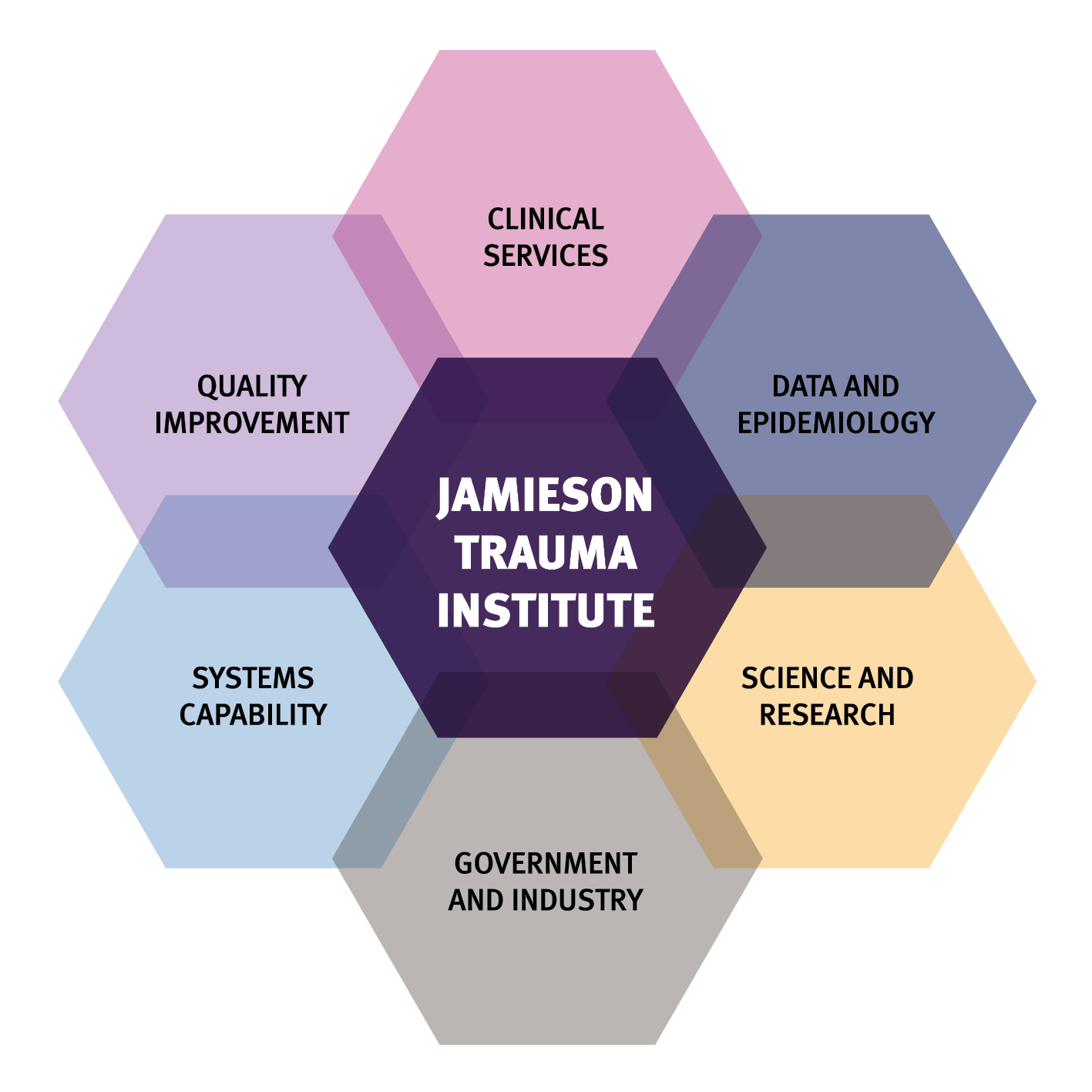
PREdiction and Diagnosis using Imaging and Clinical biomarkers Trial in Traumatic Brain Injury (PREDICT-TBI) is a prospective, longitudinal, observational, multicentre study for patients who have suffered a moderate or severe TBI. PREDICT-TBI was born from the partnership of Associate Professor Fatima Nasrallah and Associate Professor Cliff Pollard (Jamieson Trauma Institute), who jointly set out to build the team and gather the resources needed to kick off the study.
The overall aim of PREDICT-TBI, is to use machine learning and determine and compare the univariate and multivariate associations between neuroimaging biomarkers, blood biomarkers, clinical data and neurological outcomes in adults with moderate to severe TBI. The specific aims are:
- To identify neuroimaging biomarkers of TBI, measured as structural and functional damage on brain MRI, following discharge from ICU/HDU (or if not admitted to ICU, once the participant is stable on the ward) and changes in structural damage and neuro-inflammation during recovery at 3- and 6-months after injury.
- To determine the multivariate associations between neuroimaging biomarkers of TBI and neurological outcomes 3- and 6-months after injury, using a combination of deep learning and other machine learning methodologies.
- To determine correlations between neuroimaging biomarkers, blood biomarkers (ccfDNA, exosomes), clinical data and neurological outcomes of TBI on discharge from ICU and at 3- and 6-months after injury.
- To determine correlations between 3-month and 6-month changes in neuroimaging biomarkers, blood biomarkers, clinical data and neurological outcomes.
- To determine the independent predictors of neurological outcomes at 3- and 6-months after injury using deep learning.
- To assess aims 2-4 in the subgroup of patients who have MRI scans (during their ICU/HDU admission) as part of their clinical care.
Clinical significance
This study will provide a novel Australian-based background on the determinants of neurological outcomes in moderate-severe TBI patients. The results of this study could be the scaffold for the development of programs that incorporate evidence-based approaches to trauma care with the purpose of:
- sharing information across Australia-wide trauma centres
- increasing the consumer involvement in trauma services and
- developing patient-centred quality of care for the improvement of TBI outcomes in Australia and worldwide.
Furthermore, this study will also consolidate a pioneering collaboration between the Jamieson Trauma Institute, the Queensland Brain Institute, the Australian Institute for Bioengineering and Nanotechnology, The University of Queensland, the Herston Imaging Research Facility and CSIRO with clinicians for the development of research platforms that ultimately should benefit patient care.
We aim to recruit 300 participants from the following sites in Queensland, New South Wales, Victoria and The Northern Territory:
- Royal Brisbane and Women’s Hospital, Brisbane
- Princess Alexandra Hospital, Brisbane
- Royal Darwin Hospital, Darwin
- Liverpool Hospital, Sydney
- Gold Coast University Hospital, Southport
- Townsville University Hospital, Townsville
- The Alfred Hospital, Melbourne
Inclusion criteria
- Aged ≥ 18 years old
- Diagnosed with moderate or severe TBI*, with or without other injuries.
*TBI Definition – A TBI will be defined based on the post-resuscitation Glasgow Coma Scale (GCS) in the pre-hospital period and the first 24 hours of ICU admission, if admitted to ICU. Moderate and Severe TBI are defined by the following categories of GCS if in the opinion of the treating team GCS is not solely due to intoxication, sedation, or extracranial injury.
- Moderate TBI is defined as a GCS score of 9-12
- Severe TBI is defined as a GCS score of ≤8
Exclusion criteria
- Previous major stroke
- Pregnancy, or may be pregnant
- In the opinion of the investigator the participant would be unlikely to be able to comply with study procedures and follow up (e.g. lives overseas).
- Presence of underlying disease with a life expectancy of less than 6 months
- Known contraindication to MRI that will prevent study procedures
- Patients who have suffered a devastating TBI with either progression towards brain death at the time of assessment or where the treating medical team are not committed to ongoing full supportive care
- Traumatic brain injury occurred more than 72 hours ago
1. Neuroimaging
- Post ICU discharge
- 3-month post injury
- 6-month post injury
2. Blood sample biomarkers
- Within 36 hours post injury
- Between 48 and 72 hours post injury
- Day 4 post injury +/- 24hours
- Day 7 post injury +/- 24 hours
- Day 14 post injury +/- 24hours
- 3 months post injury.
3. Neurological outcome measures at 3 months post-injury
- Brief Resilience Scale (BRS)
- Generalized Anxiety Disorder 7-item Scale (GAD - 7)
- Glasgow Outcome Scale – Extended (GOS-E)
- Patient Reported Outcomes Measurement Information System (PROMIS)
- Post-Traumatic Stress Disorder Checklist (PCL-5)
- Patient Health Questionnaire (PHQ-15)
- Patient Health Questionnaire (PHQ-9)
4. Neurological outcome measures at 6 months post-injury
- Brief Resilience Scale (BRS)
- Generalized Anxiety Disorder 7-item Scale (GAD - 7)
- Glasgow Outcome Scale – Extended (GOS-E)
- Patient Reported Outcomes Measurement Information System (PROMIS)
- Post-Traumatic Stress Disorder Checklist (PCL-5)
- Patient Health Questionnaire (PHQ-15)
- Patient Health Questionnaire (PHQ-9)
- Barry Rehabilitation Inpatient Screening of Cognition (BRISC) Scale
Lead investigators
Associate Professor Fatima Nasrallah A/Professor Nasrallah is a neuroscientist with a background in magnetic resonance and interdisciplinary brain research. She graduated with a PhD in neurochemistry and NMR from the Neuroscience Research Australia Institute (NeurRA) at the University of New South Wales in 2009. In April 2009, She spent 3 years at the Singapore Bioimaging Consortium (A*STAR) where she pioneered the use of magnetic resonance imaging as a tool in cognitive brain research in the rodent. In 2013, she was appointed as senior research fellow at the Clinical Imaging Research Center where she delved into the clinical realms of human imaging. In late 2015, she returned to Australia as a Motor Accident and Injury Commission fellow at the Queensland Brain Institute (QBI) at the University of Queensland (UQ) where she independently heads her own group. Her research spans basic and clinical brain research with the the overall aim of understanding how the brain functions in health and injury, specifically, developing methods for early diagnosis of primary biomarkers following injury and translating these findings.
A/Professor Nasrallah is a neuroscientist with a background in magnetic resonance and interdisciplinary brain research. She graduated with a PhD in neurochemistry and NMR from the Neuroscience Research Australia Institute (NeurRA) at the University of New South Wales in 2009. In April 2009, She spent 3 years at the Singapore Bioimaging Consortium (A*STAR) where she pioneered the use of magnetic resonance imaging as a tool in cognitive brain research in the rodent. In 2013, she was appointed as senior research fellow at the Clinical Imaging Research Center where she delved into the clinical realms of human imaging. In late 2015, she returned to Australia as a Motor Accident and Injury Commission fellow at the Queensland Brain Institute (QBI) at the University of Queensland (UQ) where she independently heads her own group. Her research spans basic and clinical brain research with the the overall aim of understanding how the brain functions in health and injury, specifically, developing methods for early diagnosis of primary biomarkers following injury and translating these findings.
Professor Michael Reade
 Professor Reade was appointed Head of the Mayne Academy of Critical Care at the University of Queensland in 2021, with oversight of teaching and research in anaesthetics, intensive care and emergency medicine across the 11 clinical units of the university. He continues to lead the expanding Australian Defence Force trauma research program based at UQ, covering trauma systems design, blood and fluid resuscitation in trauma, and traumatic brain injury. His frozen platelet trial program, conducted with the Australian Red Cross, aims to improve worldwide access to this vital component of trauma resuscitation. Professor Reade is also developing a research programme focussed on trauma systems design, in collaboration with colleagues at the Jamieson Trauma Institute on the Royal Brisbane and Women's Hospital campus, Australian state ambulance services and the US and UK armed forces, aiming (for example) to optimise the allocation of prehospital and hospital resources in the management of life-threatening trauma. He works clinically as an intensivist at the Royal Brisbane and Women’s Hospital.
Professor Reade was appointed Head of the Mayne Academy of Critical Care at the University of Queensland in 2021, with oversight of teaching and research in anaesthetics, intensive care and emergency medicine across the 11 clinical units of the university. He continues to lead the expanding Australian Defence Force trauma research program based at UQ, covering trauma systems design, blood and fluid resuscitation in trauma, and traumatic brain injury. His frozen platelet trial program, conducted with the Australian Red Cross, aims to improve worldwide access to this vital component of trauma resuscitation. Professor Reade is also developing a research programme focussed on trauma systems design, in collaboration with colleagues at the Jamieson Trauma Institute on the Royal Brisbane and Women's Hospital campus, Australian state ambulance services and the US and UK armed forces, aiming (for example) to optimise the allocation of prehospital and hospital resources in the management of life-threatening trauma. He works clinically as an intensivist at the Royal Brisbane and Women’s Hospital.
Dr James Walsham
 Dr James Walsham is a senior Intensive Care Specialist and Director of Research at the Princess Alexandra Hospital. Dr Walsham graduated from Manchester University (UK) in 1994 and following completion of the Membership of the Royal College of Physicians exams moved to Australia and completed Intensive Care training in South-East Queensland. Since commencing as a specialist in 2007 Dr Walsham has practiced at the Princess Alexandra Hospital as well being exposed to Metropolitan ICU at Ipswich Hospital and private practice at Greenslopes Private Hospital. From early on in his specialist career he has been involved in research, setting up infrastructure to facilitate participation in multicentre trials in Ipswich ICU and subsequently being appointed Director of Research at Princess Alexandra in 2016, where Dr Walsham drives the Intensive Care research program with participation in multiple trials. He is currently leading the FluDReSS trial assessing fludrocortisone in septic shock patients as well as a trial investigating the EM Vision portable brain imaging device in stroke patients.
Dr James Walsham is a senior Intensive Care Specialist and Director of Research at the Princess Alexandra Hospital. Dr Walsham graduated from Manchester University (UK) in 1994 and following completion of the Membership of the Royal College of Physicians exams moved to Australia and completed Intensive Care training in South-East Queensland. Since commencing as a specialist in 2007 Dr Walsham has practiced at the Princess Alexandra Hospital as well being exposed to Metropolitan ICU at Ipswich Hospital and private practice at Greenslopes Private Hospital. From early on in his specialist career he has been involved in research, setting up infrastructure to facilitate participation in multicentre trials in Ipswich ICU and subsequently being appointed Director of Research at Princess Alexandra in 2016, where Dr Walsham drives the Intensive Care research program with participation in multiple trials. He is currently leading the FluDReSS trial assessing fludrocortisone in septic shock patients as well as a trial investigating the EM Vision portable brain imaging device in stroke patients.
Dr Judith Bellapart
 Dr Judith Bellapart is a senior intensive care specialist with a specific interest in neurocritical care. She is an intensivist trained at the University of Barcelona (1996-2000) and awarded with a research scholarship on the field of cerebral vasospasm in subarachnoid hemorrhage at Saint Michael’s Hospital, University of Toronto, Canada from 2002 to 2004. Since 2007, she has been a full-time specialist at a tertiary university hospital and trauma centre, The Royal Brisbane and Women’s Hospital, in Queensland and a Fellow of the College of Critical Care Medicine, Australia. Dr Bellapart has conducted a series of research studies focused on the assessment of cerebral autoregulation in critically ill patients under quaternary cardiac support such as Intra-aortic balloon pumps, Ventricular Assist Devices and Extracorporeal circulation. She has been a principal site investigator in several national and international neuro-critical care randomised trials in the field of Subarachnoid hemorrhage, such as the Conscious I and Conscious II Trials. She has been the CI on a multicentre study based on the diagnostic sensitivity of Endothelin-1A in plasma for symptomatic vasospasm after subarachnoid hemorrhage. She completed a higher research degree (PhD) by the University of Queensland, with a series of experimental studies assessing the effect of normovolemic anemia on cerebral microcirculation after severe head injury. She is a regular reviewer for Intensive Care Medicine and Frontiers in Neurology. Between 2009 – 2019 she was the coordinator of the accredited Transcranial Doppler course, focusing on the assessment of cerebral hemodynamics in neurocritical patients. Dr Bellapart has been the recipient for grants from the Research foundation, Defence Health Foundation and Brain Foundation. Currently, she is a CI for PREDICT-TBI - Prediction and Diagnosis using Imaging and Clinical biomarkers Trial in Traumatic Brain Injury.
Dr Judith Bellapart is a senior intensive care specialist with a specific interest in neurocritical care. She is an intensivist trained at the University of Barcelona (1996-2000) and awarded with a research scholarship on the field of cerebral vasospasm in subarachnoid hemorrhage at Saint Michael’s Hospital, University of Toronto, Canada from 2002 to 2004. Since 2007, she has been a full-time specialist at a tertiary university hospital and trauma centre, The Royal Brisbane and Women’s Hospital, in Queensland and a Fellow of the College of Critical Care Medicine, Australia. Dr Bellapart has conducted a series of research studies focused on the assessment of cerebral autoregulation in critically ill patients under quaternary cardiac support such as Intra-aortic balloon pumps, Ventricular Assist Devices and Extracorporeal circulation. She has been a principal site investigator in several national and international neuro-critical care randomised trials in the field of Subarachnoid hemorrhage, such as the Conscious I and Conscious II Trials. She has been the CI on a multicentre study based on the diagnostic sensitivity of Endothelin-1A in plasma for symptomatic vasospasm after subarachnoid hemorrhage. She completed a higher research degree (PhD) by the University of Queensland, with a series of experimental studies assessing the effect of normovolemic anemia on cerebral microcirculation after severe head injury. She is a regular reviewer for Intensive Care Medicine and Frontiers in Neurology. Between 2009 – 2019 she was the coordinator of the accredited Transcranial Doppler course, focusing on the assessment of cerebral hemodynamics in neurocritical patients. Dr Bellapart has been the recipient for grants from the Research foundation, Defence Health Foundation and Brain Foundation. Currently, she is a CI for PREDICT-TBI - Prediction and Diagnosis using Imaging and Clinical biomarkers Trial in Traumatic Brain Injury.
Professor Andrew Udy
 Andrew is a full-time intensive care clinician and researcher at The Alfred ICU, Melbourne. He completed his undergraduate medical education at the University of Auckland, followed by ICU training in New Zealand, the United Kingdom and Australia. After award of Fellowship, Andrew worked as a consultant for many years in Queensland, while also completing a PhD in antibiotic pharmacokinetics. His major academic interests include optimised drug prescribing in the critically ill, haemodynamic management in severe sepsis, acute kidney injury and renal replacement therapy, management of SAH and TBI, and critical care nutrition. Andrew is involved in critical care research internationally as an Executive Member of the ANZICS Clinical Trials Group (CTG). He also a keen educator; instructing on BASIC, ALS, ECMO, ENLS and EMST courses, and is Chair of the Neurocritical Care Special Interest Group, College of Intensive Care Medicine. Andrew is Co-Deputy Director of the Australian and New Zealand Intensive Care – Research Centre, Monash University.
Andrew is a full-time intensive care clinician and researcher at The Alfred ICU, Melbourne. He completed his undergraduate medical education at the University of Auckland, followed by ICU training in New Zealand, the United Kingdom and Australia. After award of Fellowship, Andrew worked as a consultant for many years in Queensland, while also completing a PhD in antibiotic pharmacokinetics. His major academic interests include optimised drug prescribing in the critically ill, haemodynamic management in severe sepsis, acute kidney injury and renal replacement therapy, management of SAH and TBI, and critical care nutrition. Andrew is involved in critical care research internationally as an Executive Member of the ANZICS Clinical Trials Group (CTG). He also a keen educator; instructing on BASIC, ALS, ECMO, ENLS and EMST courses, and is Chair of the Neurocritical Care Special Interest Group, College of Intensive Care Medicine. Andrew is Co-Deputy Director of the Australian and New Zealand Intensive Care – Research Centre, Monash University.
Associate Professor Dennis Cordato
 Associate Professor Dennis Cordato is a Staff Specialist Neurologist at Liverpool Hospital and the Academic Head of Stroke and Neurology Research at the Ingham Institute of Applied Medical Research. He has been a Staff Specialist Neurologist in South Western Sydney for over 20 years and has been actively involved in clinical research since completing his own PhD in neuropharmacology in 2001. He has a strong interest in clinical stroke research and has been the principal investigator at Liverpool Hospital in multiple acute and post-acute stroke trials including ischaemic and hemorrhagic stroke. He leads a research team of clinical trials coordinators, research assistants and medical, nursing and allied health colleagues with a focus on acute stroke interventions in particular thrombolysis and endovascular clot retrieval. Over the years, Associate Professor Cordato has supervised a number of PhD, Masters and Honours students as well as medical students to complete theses and projects in the areas of stroke and neurology. The SWS STRONG team at Liverpool Hospital is excited to be involved in PREDICT-TBI and looks forward to contributing to this worthwhile project that will hopefully shed important new lights into how the brain functions following injury.
Associate Professor Dennis Cordato is a Staff Specialist Neurologist at Liverpool Hospital and the Academic Head of Stroke and Neurology Research at the Ingham Institute of Applied Medical Research. He has been a Staff Specialist Neurologist in South Western Sydney for over 20 years and has been actively involved in clinical research since completing his own PhD in neuropharmacology in 2001. He has a strong interest in clinical stroke research and has been the principal investigator at Liverpool Hospital in multiple acute and post-acute stroke trials including ischaemic and hemorrhagic stroke. He leads a research team of clinical trials coordinators, research assistants and medical, nursing and allied health colleagues with a focus on acute stroke interventions in particular thrombolysis and endovascular clot retrieval. Over the years, Associate Professor Cordato has supervised a number of PhD, Masters and Honours students as well as medical students to complete theses and projects in the areas of stroke and neurology. The SWS STRONG team at Liverpool Hospital is excited to be involved in PREDICT-TBI and looks forward to contributing to this worthwhile project that will hopefully shed important new lights into how the brain functions following injury.
Associate Professor Lewis Campbell
 A/Professor Campbell is an Intensive Care physician and director of research at Royal Darwin Hospital, working closely with Flinders University, Charles Darwin University, and Menzies School of Health Research. He has been the site investigator for multisite trials in sedation practice, sepsis, brain injury, community acquired pneumonia, and Covid-19. His contribution to research in the Northern Territory has largely been in healthcare research policy and governance, and he is the NT representative on the inter jurisdictional working groups relating to ethics review, site specific assessment and governance of research. In these roles he has collaborated in projects to embed the practice of research into routine care, and to smooth the process of translation of research evidence into routine care practice. He is Chair Emeritus of the NT Health Research Ethics Committee and was instrumental in the inclusion of the NT in the National Mutual Acceptance scheme. He leads educational and practice initiatives on encouraging and embedding research into care.
A/Professor Campbell is an Intensive Care physician and director of research at Royal Darwin Hospital, working closely with Flinders University, Charles Darwin University, and Menzies School of Health Research. He has been the site investigator for multisite trials in sedation practice, sepsis, brain injury, community acquired pneumonia, and Covid-19. His contribution to research in the Northern Territory has largely been in healthcare research policy and governance, and he is the NT representative on the inter jurisdictional working groups relating to ethics review, site specific assessment and governance of research. In these roles he has collaborated in projects to embed the practice of research into routine care, and to smooth the process of translation of research evidence into routine care practice. He is Chair Emeritus of the NT Health Research Ethics Committee and was instrumental in the inclusion of the NT in the National Mutual Acceptance scheme. He leads educational and practice initiatives on encouraging and embedding research into care.
Mark Sheridan
James McCullough
Siva Senthuran
Clinical trial manager
Dr Tracey Evans
 Tracey is the PREDICT-TBI Clinical Trial Manager at the Queensland Brain Institute,The University of Queensland (UQ). She completed her PhD at UQ where her research focused on the quality of a mother’s bonding with her infant following a very preterm birth. Tracey also investigated the effects of the very preterm birth on maternal responsiveness, self-efficacy, depressive symptoms, and trauma symptoms. Previous to her position on the PREDICT-TBI study, Tracey managed infant research studies for the Queensland Cerebral Palsy Rehabilitation and Research Centre (UQ) at the Centre for Children’s Health Research, and for the Australian Catholic University at the Mater Mothers’ Hospital. Through these positions, Tracey gained extensive experience in research management of state, national and international studies, including ethics and governance applications, data storage and management, stakeholder engagement, database construction, project documentation and staff education and training. Tracey has also worked as a Registered Nurse in all areas of nursing, including neurological and neurosurgical intensive care.
Tracey is the PREDICT-TBI Clinical Trial Manager at the Queensland Brain Institute,The University of Queensland (UQ). She completed her PhD at UQ where her research focused on the quality of a mother’s bonding with her infant following a very preterm birth. Tracey also investigated the effects of the very preterm birth on maternal responsiveness, self-efficacy, depressive symptoms, and trauma symptoms. Previous to her position on the PREDICT-TBI study, Tracey managed infant research studies for the Queensland Cerebral Palsy Rehabilitation and Research Centre (UQ) at the Centre for Children’s Health Research, and for the Australian Catholic University at the Mater Mothers’ Hospital. Through these positions, Tracey gained extensive experience in research management of state, national and international studies, including ethics and governance applications, data storage and management, stakeholder engagement, database construction, project documentation and staff education and training. Tracey has also worked as a Registered Nurse in all areas of nursing, including neurological and neurosurgical intensive care.
Site staff
Royal Brisbane and Women's Hospital
- Michael Reade – Lead Site Investigator
- Judith Bellapart – Lead Site Investigator
- Janine Stuart – Research Coordinator
- Melissa Lassig-Smith – Research Coordinator
- Lynn Murray – Research Coordinator
- Amelia Livermore – Research Coordinator
- Georgina Peacock – Research Coordinator
Princess Alexandra Hospital
- James Walsham – Lead Site Investigator
- Jason Meyer – Research Coordinator
- Meg Harwood – Research Coordinator
- Josephine Mackay – Research Coordinator
- Niki McGuiness– Research Coordinator
- Megan Davis – Research Coordinator
Royal Darwin Hospital
- Lewis Campbell – Lead Site Investigator
- Mary Ann Tiras – Research Coordinator
Liverpool Hospital
- Dennis Cordato – Lead Site Investigator
- Jordan Rogers – Research Coordinator
Gold Coast University Hospital
- James McCullough – Lead Site Investigator
- Mandy Tallot – Research Coordinator
- Elizabeth Wake – Research Coordinator
- Maree Houbert – Research Coordinator
- Julie Pitman – Research Coordinator
Townsville University Hospital
- Siva Senthuran – Lead Site Investigator
- Karen Carson – Research Coordinator
- Monica Watson – Research Coordinator
Alfred Hospital
- Andrew Udy – Lead Site Investigator
- Jasmine Board – Research Coordinator
- Laura Adams – Research Coordinator
The information provided here has been designed to help the person who had the brain injury, and those around them, to understand:
- why you were recruited to PREDICT-TBI
- what assessments you completed for the study - for people who have already participated in the study
- useful tips to help you when completing the assessments - for people who are still participating in the study
When you click on a heading it will expand to show the information relating to each topic. You can click on the heading again to collapse it.
Why you were recruited to PREDICT-TBI
PREDICT-TBI is a research study that aims to improve doctors’ ability to predict recovery following a traumatic brain injury (TBI).
You were recruited because you were admitted to hospital after suffering a TBI.
Participation in this study was voluntary, and either you or a Substitute Decision Maker if you were not well enough, signed a consent form to allow you to take part in this research.
Your participation is important, as understanding recovery following a TBI may allow improved early treatment and rehabilitation for people in the future who have had an injury similar to yours.
What was involved with your blood samples
About a tablespoon (25mls) of blood was taken up to 6 times in the 3 months following your injury:
- Within 36 hours of your injury
- Between 48 and 72 hours after your injury
- Four days after your injury
- Seven days after your injury
- Fourteen days after your injury (or until you were discharged from the hospital if it was earlier than 14 days following the injury)
- Three months after your injury (if you were already discharged from hospital, you were contacted to arrange a time that was convenient to return to the hospital for the sample to be taken). If you had a study MRI scan at three months, bloods were taken on the same day.
What was involved with your Magnetic Resonance Imaging (MRI) scans
You underwent MRI scans up to three times during the six months following your injury:
- Close to the time you were discharged from the Intensive Care Unit or were transferred to a ward bed
- Three months after your injury
- Six months after your injury
The MRIs were either done at the hospital which treated you, or they were organised to be done somewhere else that was suitable.
What was involved with the questions about your recovery
You were asked to answer some questions about your recovery two times during the six months following your injury:
- Three months after your injury
- Six months after your injury
These were done either face to face or over the phone at a time that was convenient to you.
Helpful tips and information for people still participating in the study
- The blood samples are collected by trained and qualified staff.
- The study blood draws will coincide with routine clinical blood draws whenever possible.
- The MRI can take some time to set up and complete. Going to the toilet before the scan commences can make it a more comfortable experience.
- The MRI scanning machine makes loud tapping sounds when in operation. Disposable earplugs will be provided to reduce the noise to a tolerable level, and if available, music or other audio distraction measures will be provided.
- The lighting will be dimmed for comfort during the MRI, and you will be provided with a buzzer if you need to communicate with the staff.
- MRIs will be organised to coincide with your follow up outpatients’ appointments, when possible, to minimise the number of visits to the hospital.